ACL Reconstruction Surgery
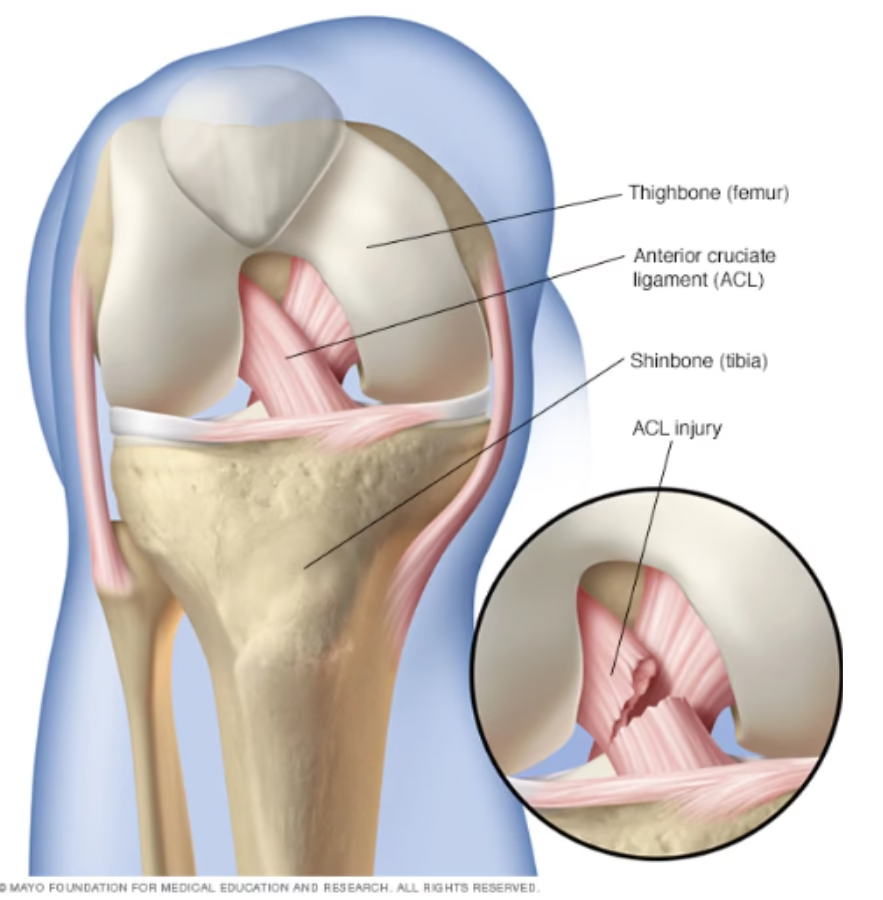
The ACL (anterior cruciate ligament) keeps your knee steady during twisting and turning. When it tears, the knee may swell, feel unstable, or “give way.” ACL reconstruction replaces the torn ligament with a strong graft to restore stability so you can return to daily life and sport safely.
Written for patients in simple language. Evidence-based, minimally invasive approach.
What is the ACL and why does it matter?
The ACL is one of four key knee ligaments. It connects your thigh bone (femur) to your shin bone (tibia) and prevents the shin from sliding too far forward. It also controls rotational stability. Without a healthy ACL, the knee can feel loose or buckle during sudden moves.
How does an ACL tear happen?
Most tears occur during a quick change of direction, sudden stop, or awkward landing from a jump—often in football, basketball, badminton, or running. Many people hear a “pop,” the knee swells, and walking feels unstable. Meniscus (cartilage) injuries can happen at the same time.
Do you always need surgery?
Not everyone needs an operation. Some people—especially with lower activity demands—do well with physiotherapy, bracing, and activity changes. Surgery is usually recommended if:
- Your knee repeatedly “gives way” in daily life
- You wish to return to sport or physically demanding work
- There are associated injuries (meniscus or cartilage) that need repair
- Non-surgical treatment has not restored stability
Decision-making is personalized after clinical exam, MRI, your goals, and activity level. You and your surgeon choose the safest, most effective plan.
How ACL reconstruction surgery is done
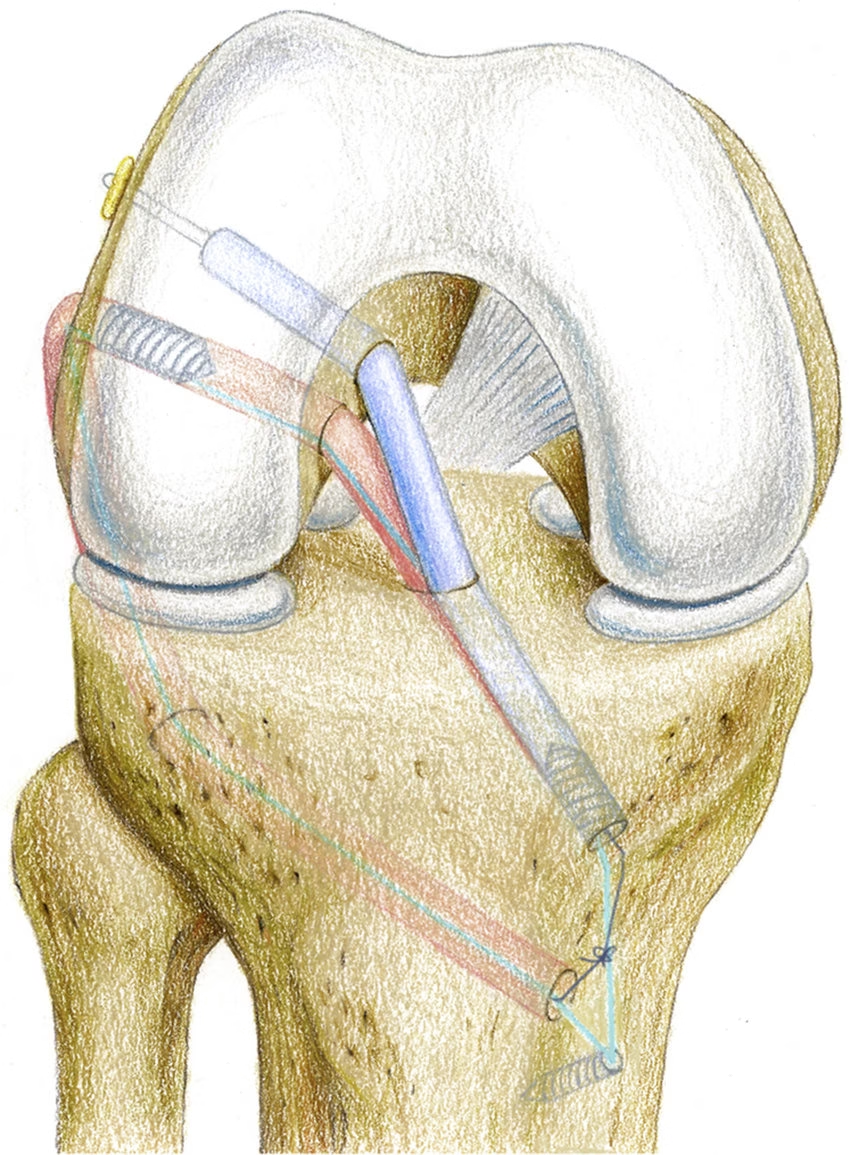
The procedure is arthroscopic (keyhole). Through small incisions, the torn ligament is replaced with a tendon graft and fixed securely so it can heal as a new “ligament.”
- Remove damaged ACL tissue
- Choose a graft (hamstring, patellar tendon, quadriceps; special cases may use donor tissue)
- Drill precise tunnels in femur and tibia
- Pass the graft, tension it correctly, and fix it with implants
- Close incisions and begin early rehabilitation
Graft options—what’s best for you?
- Hamstring graft — common, smaller incision, strong
- Bone-patellar tendon-bone (BTB) — strong fixation; may have front-of-knee tenderness in some
- Quadriceps tendon — good option for certain knees or revisions
- Allograft (donor) — selected cases; pros and cons discussed individually
Your surgeon will match the graft to your sport, knee anatomy, and recovery goals.
Recovery & rehabilitation timeline (typical)
Every knee heals at its own pace. This roadmap shows common milestones; your plan is individualized.
| Phase | Goals & activities |
|---|---|
| 0–2 weeks | Control swelling, achieve full knee straightening, gentle quadriceps activation, walk with crutches as advised. |
| Weeks 3–6 | Increase knee bend, progressive weight-bearing, start strengthening and balance work. |
| Months 3–6 | Advance strength, agility, low-impact sport drills, functional training. |
| 6–12+ months | Sport-specific training, cutting/pivot drills, return to competition once strength & functional tests are passed. |
Before surgery: helpful tips
- Work on gentle range-of-motion to avoid stiffness (as guided)
- Strengthen quadriceps and hamstrings safely
- Avoid twisting/pivoting; consider brace/crutches to prevent further injury
Expected outcomes & possible risks
Most patients regain knee stability and return to active life with proper surgery and rehab. As with any operation, risks include graft re-tear, stiffness, infection, or persistent pain. Careful technique, adherence to physiotherapy, and realistic goals reduce these risks.
Frequently asked questions
When can I walk normally?
Usually within days with support; full weight-bearing progresses as swelling and pain settle and your surgeon approves.
How long until I play sports again?
Many return between 9–12 months, after passing strength, balance, and functional tests. Timelines vary per knee and sport.
Will my knee feel the same as before?
Many patients feel close to “normal.” Minor differences can persist, but with good rehab, most people adapt very well.
Have MRI reports? Bring them along for a personalized plan.
